Exercise & Diabetes Management

Carter Bailey
Exercise Physiologist
- 6 October, 2025
- Exercises Medicine
- Exercise Physiology
- 3 min read
Exercise & Diabetes Management
Diabetes refers to a group of chronic metabolic diseases characterised by hyperglycaemia (high blood glucose) resulting from defects in insulin secretion, insulin action, or both. It is a growing public health concern: in the UK, an estimated 5.6 million people are living with diabetes, equivalent to about 7% of the population. The condition places a significant burden on healthcare resources, with the NHS spending at least £10 billion annually on diabetes care, around 80% of which is devoted to treating complications.
The most common form is type 2 diabetes, which accounts for around 90% of all cases. It arises from a combination of reduced insulin secretion by the pancreas, limiting the body’s ability to regulate blood glucose levels, and insulin resistance, which leads to increased glucose production in the liver and reduced glucose uptake by muscle and fat tissue. Risk factors for type 2 diabetes include family history, age, and ethnicity, as well as modifiable factors such as obesity, physical inactivity, smoking, high blood pressure, abnormal blood lipids, and poor diet.
About 8% of cases are type 1 diabetes, a chronic autoimmune condition in which the immune system destroys the insulin-producing cells of the pancreas. This results in absolute insulin deficiency and persistent hyperglycaemia. Although type 1 diabetes can occur at any age, it is most often diagnosed in children and adolescents. Management requires lifelong insulin therapy and regular blood glucose monitoring.
Other, less common forms of diabetes include gestational diabetes, which develops during pregnancy, and rare types linked to genetic mutations, pancreatic disease, or certain medications.
Without proper management of glucose levels, diabetes can lead to serious complications, including nerve damage (neuropathy), cardiovascular disease, kidney disease, eye conditions such as retinopathy, and musculoskeletal problems. Effective management through lifestyle changes, medication, and regular monitoring can help reduce the risk of these complications and improve quality of life.
Exercise is Essential
Exercise is a cornerstone of diabetes management, providing numerous benefits for people with both type 1 and type 2 diabetes. Regular physical activity increases energy expenditure, helping to reduce visceral and subcutaneous fat, while promoting muscle growth and improving glucose storage. It also increases glucose uptake by skeletal muscles independently of insulin and boosts insulin sensitivity in muscle, fat, and liver for up to 72 hours, supporting better blood glucose control. Beyond metabolic benefits, exercise increases cardiovascular fitness, improves heart and blood vessel function, and positively impacts key risk factors such as blood pressure and cholesterol levels, collectively lowering the risk of cardiovascular disease and premature mortality.
Key Considerations
For individuals with diabetes, exercising safely requires some important considerations. People with type 1 diabetes or those taking medications that increase insulin secretion are at risk of hypoglycaemia (low blood sugar), so regular blood glucose monitoring is essential.
The structure of an exercise session can also help lower this risk. Research suggests that performing resistance training before aerobic exercise or including short, high-intensity intervals during moderate-intensity aerobic sessions can help prevent blood glucose drops. Timing matters too, early morning exercise may sometimes raise blood glucose instead of lowering it, as is typical with moderate activity.
Choosing the right intensity is crucial, since very vigorous exercise can also cause temporary blood sugar elevations. Whenever possible, supervised exercise is recommended to minimise risks and safely manage any hypoglycaemic events.

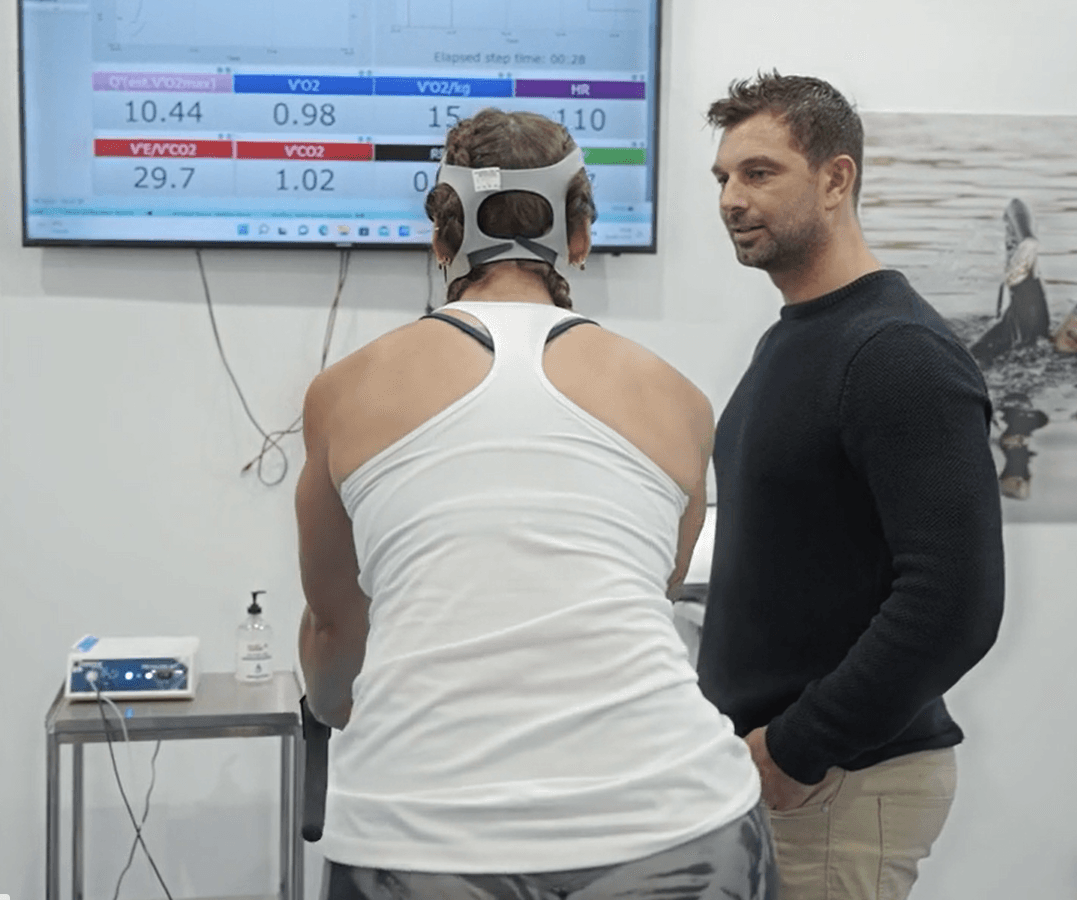
Why Work with an Exercise Physiologist
People with diabetes benefit significantly from working with an Exercise Physiologist. We provide personalised, safe, and effective exercise programs tailored to an individual’s type of diabetes, medications, fitness level, and any existing complications. Our structured plans are designed to reduce the risk of hypoglycaemia and injury, while improving cardiovascular health, increasing insulin sensitivity, supporting weight management, and helping prevent complications such as neuropathy or heart disease.
Beyond exercise prescription, Exercise Physiologists offer education, motivation, and ongoing support, empowering people with diabetes to safely incorporate physical activity into their daily lives and improve overall health and wellbeing.

Advice
Over the last 20+ years our experts have helped more than 100,000 patients, but we don’t stop there. We also like to share our knowledge and insight to help people lead healthier lives, and here you will find our extensive library of advice on a variety of topics to help you do the same.
OUR ADVICE HUBS See all Advice Hubs

