Effective Strategies for Managing Various Headache Types: Part 2

Pure Sports Medicine
- 8 December, 2020
- Neurology
- 5 min read
Effective Strategies for Managing Various Headache Types: Part 2

Physiotherapy is often involved in the management of headaches, but how do we know if it is effective?
Two important things to consider when answering this question are, how is effectiveness defined, and does the headache type impact the effectiveness of physiotherapy treatment?
There are many different variables to consider when determining if treatment is effective. These may include headache intensity, duration, frequency, as well as response or need for medication. Ultimately, these variables are trying to capture if treatment has had a meaningful effect on the individual.
Research evidence shows us that:
- Different types of headache may have different underlying mechanisms driving headache symptoms. (4-6) Differentiating between headache types is therefore a crucial first step in developing a management plan. (1, 4, 5)
- Depending on headache type, Physiotherapy may be the main treatment approach or it may be used in combination with other treatments, for example, alongside medication or cognitive behavioural therapy (CBT). (1, 7)
- Physiotherapy interventions differ slightly between studies and can include joint mobilisations, trigger point pressure and exercise. (1)
- Physiotherapy treatment is effective for individuals with cervicogenic headaches (headaches originating from the neck). (9, 10)
- The strongest evidence for this, is the positive effect it has on reducing the pain’s intensity. There is also improvement in the frequency and duration of the headaches, as well as a reduction in functional disability.
- Physiotherapy may also have a positive effect on the intensity, duration and frequency of migraines, and the intensity of tension-type headaches (TTHs). Whether these statistically significant changes represent a meaningful change should be considered in relation to the time and cost of the treatment approach. (1)
- In some studies, interventions for the treatment of TTH and migraine seem to be based on theory and beliefs, rather than individual impairments identified during assessment. (1)
- Research exploring the role of sustained mobilisations – such as continued pressure on on the neck, as shown in the image above – in the treatment of individuals with mixed headache forms, including migraine, have shown promise. (6, 8) Further research with larger sample sizes will help determine how effective this treatment approach is, and if it is effective in all types of migraine. (6)
Physiotherapy Assessment
The main aims of an initial assessment with a Physiotherapist, are to:
- Identify headache type and any red flags which may suggest the presence of a secondary headache
- Establish outcome measures to track progress and determine treatment effectiveness
- Recognise potential headache triggers which may be contributing to the development of symptoms (e.g. poor lifting technique at the gym, stress, prolonged screen use, poor sleep – quantity or quality)
- Identify impairments which can be targeted in treatment (e.g. neck muscle weakness)
Headache type is diagnosed based on symptoms, and the findings from a clinical physical examination. (2) During a physical examination, the recreation and resolve of a headache when applying sustained pressure over the upper neck segments, would suggest a link between the neck and the headache. (6, 11)
Additional signs of neck dysfunction identified during an assessment may include, poor movement control, muscle weakness, hypomobility, or ‘stiffness’ of the upper neck joints and the presence of trigger points. (2, 6)
These findings, together with triggers identified in the your history, provide potential targets for treatment.
Treatment
Treatment will depend on several factors including:
- Type of headache
- Severity
- Impact of headache (effect on function)
- Patient treatment preference
- Impairments identified during assessment
For some, managing a headache may consist of just avoiding triggers – weighing up if that extra glass of red wine is worth the headache in the morning – while for others, a multi-disciplinary approach involving a GP, Consultant, Physiotherapist, Psychologist, Neurologist or Pain Specialist may be required to achieve the best result.
As discussed in Understanding Headaches – Part 1 sensitisation of pain pathways, or increased responsiveness of the nervous system, is a common underlying mechanism in cervicogenic headache, TTH and migraine. Treatment should therefore be aimed at factors contributing to sensitisation such as neck dysfunction, stress and poor sleep. (6, 8, 12)
An individualised headache ‘profile’, which identifies and weights various factors contributing to sensitisation, could be established to help direct the most appropriate treatment(s). (6)
Below is an example of two different headache profiles – symptomatic and asymptomatic – and how different contributing factors may direct the treatment that follows.
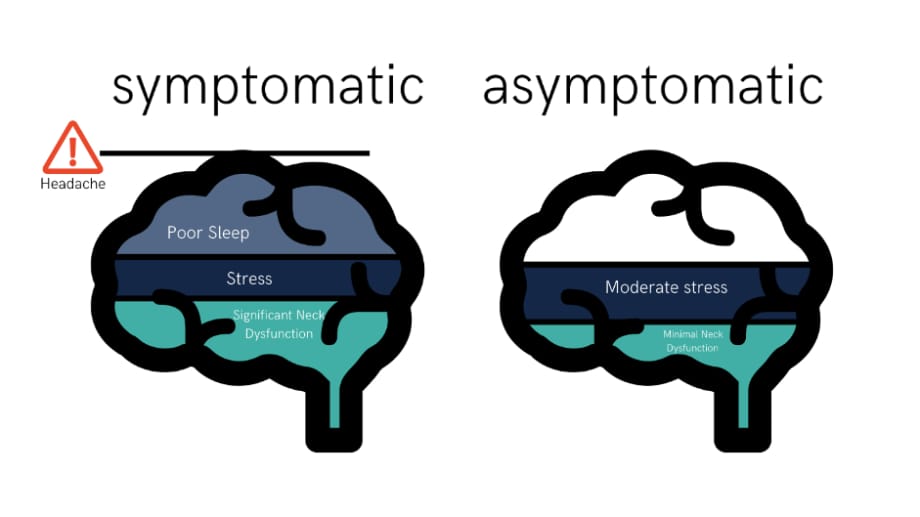
As you can see, an increase in any one factor might contribute towards reaching the threshold, but often it is a combination of different factors which results in exceeding the headache threshold. (6, 8, 11) In this example, addressing the neck component which is contributing to the headache may drop an individual below the symptomatic threshold.
If neck dysfunction is identified during the assessment, manual therapy and specific neck exercises are recommended. (6) Manual therapy, such as sustained joint mobilisations, is used to try and desensitise the structures in the neck which may be causing the headache symptoms. (6, 8, 11)
Poor control of deep neck flexor muscles has been reported in individuals with cervicogenic headache, tension-type headache and migraine. (6, 8) Furthermore, strengthening these muscles has shown to decrease symptoms in individuals with cervicogenic and TTH. (6, 10, 13)
If similar signs of weakness are found to be present in individuals with migraine, a neck strengthening program may also be beneficial. (6) Further research is needed however to determine this effect.
Psychological factors such as stress and anxiety may also contribute to sensitisation of pain pathways and the generation of headache symptoms. (12) Cognitive behavioural therapy (CBT) and mindfulness meditation are two psychological interventions which may be used to try and calm the central nervous system. (7, 14)
Sleep is essential for health and well-being and plays an important role in physical development, emotional regulation, cognitive performance and quality of life. (15)
Poor sleep is associated with increased sensitivity to pain and is often experienced by individuals living with chronic pain. (12) In athletes, better sleep may improve performance as well as reduce the risk of injury and illness. (15) Implementing good sleep habits to improve sleep quantity or quality should therefore be considered in management.
Although outside the scope of this blog, medication can also play an important role in addressing the increased responsiveness of the nervous system. Medications should only be taken when prescribed by a medical professional and may be used in combination with Physiotherapy in some cases.
To summarise, sensitisation of pain pathways (the nervous system) is a common feature in migraine, tension-type and cervicogenic headaches. Furthermore, neck dysfunction may be present in all three types.
Individualised Physiotherapy treatment can identify factors which may be contributing to sensitisation, as well as develop a rehabilitation program in order to address impairments, like neck dysfunction, that may be driving headache symptoms.
References
- Luedtke K, Allers A, Schulte LH, May A. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia : an international journal of headache. 2016;36(5):474-92.
- Hall T, Briffa K, Hopper D. Clinical evaluation of cervicogenic headache: a clinical perspective. J Man Manip Ther. 2008;16(2):73-80.
- M S, Lamont AC, Alias NA, Win MN. Red flags in patients presenting with headache: clinical indications for neuroimaging. The British journal of radiology. 2003;76(908):532-5.
- Do TP, Remmers A, Schytz HW, Schankin C, Nelson SE, Obermann M, et al. Red and orange flags for secondary headaches in clinical practice. SNNOOP10 list. 2019;92(3):134-44.
- Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia : an international journal of headache. 2018;38(1):1-211.
- Satpute K, Bedekar N, Hall T. Headache symptom modification: the relevance of appropriate manual therapy assessment and management of a patient with features of migraine and cervicogenic headache – a case report. J Man Manip Ther. 2020;28(3):181-8.
- Kamonseki DH, Lopes EP, van der Meer HA, Calixtre LB. Effectiveness of manual therapy in patients with tension-type headache. A systematic review and meta-analysis. Disability and rehabilitation. 2020:1-10.
- Watson DH, Drummond PD. Cervical referral of head pain in migraineurs: effects on the nociceptive blink reflex. Headache. 2014;54(6):1035-45.
- Rani M, Kulandaivelan S, Bansal A, Pawalia A. Physical therapy intervention for cervicogenic headache: an overview of systematic reviews. European Journal of Physiotherapy. 2019;21(4):217-23.
- Racicki S, Gerwin S, Diclaudio S, Reinmann S, Donaldson M. Conservative physical therapy management for the treatment of cervicogenic headache: a systematic review. J Man Manip Ther. 2013;21(2):113-24.
- Watson D. [Available from: https://watsonheadache.com/about-the-approach/.
- McAllister MJ. What is Central Sensitization 2013 [updated 2017. Available from: https://www.instituteforchronicpain.org/understanding-chronic-pain/what-is-chronic-pain/central-sensitization.
- Watson DH, Drummond PD. Head Pain Referral During Examination of the Neck in Migraine and Tension-Type Headache. Headache: The Journal of Head and Face Pain. 2012;52(8):1226-35.
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Ann Behav Med. 2017;51(2):199-213.
- Watson AM. Sleep and Athletic Performance. Current Sports Medicine Reports. 2017;16(6):413-8.

Advice
Over the last 20+ years our experts have helped more than 100,000 patients, but we don’t stop there. We also like to share our knowledge and insight to help people lead healthier lives, and here you will find our extensive library of advice on a variety of topics to help you do the same.
OUR ADVICE HUBS See all Advice Hubs

