The Truth Surrounding Herniated Discs

Claire Small
Chief Clinical Officer & Consultant Physiotherapist
- 18 October, 2018
- Physiotherapy
- Back Pain
- Pain Management
- 5 min read
The terminology used to describe disc related back pain can often be unhelpful in truly explaining the nature of your symptoms. Terms such as ‘slipped disc’ sound harmful, however, it is actually very normal for people to have changes to spinal discs and not have any symptoms!

Age specific prevalence estimates of degenerative spine imaging findings in asymptomatic patients:
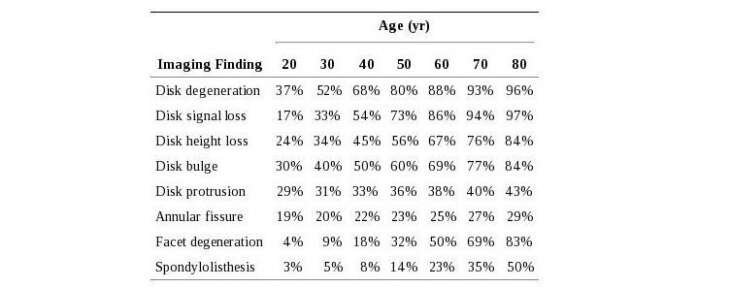
The table above shows the prevalence of changes to structures in the spine, however the patients who were studied had no symptoms. So although there may be bulging /protruding discs and several other changes present on MRI, this doesn’t always mean they are associated with a problem; in fact it is a normal age related change. It is one reason why X-rays and scans are rarely the first course of action if you present to see a doctor or other clinician with back pain.
Sometimes the nucleus may move only a small amount and stay within the disc (prolapse), or sometimes it may extend through the fibres and begin to irritate the nerves adjacent to the disc (Extrusion / Sequestration). Both small bulges and large leaking of the nuclear material can irritate a nerve, as can the inflammation that occurs as a result of the disruption. If this affects the lower fibres of the spine, it is often referred to as sciatica. Sometimes you hear people refer to any pain in the leg associated with low back pain like sciatica, but this is not truly accurate. Other structures in the low back can cause pain to radiate down the leg such as the disc itself, muscle and the facet joints.
Importantly, research has shown that the extent of your symptoms doesn’t necessarily correlate with the degree of herniation within a disc. And more importantly, the herniation does not need to reduce in size on a scan for your symptoms to resolve.
It is impossible to tell from a clinical examination, what type of disc pathology is present, especially because the type of herniation doesn’t correlate to a level of pain or the presence of nerve irritation. Remember — 10 – 81% of individuals with no pain, will have some kind of disc pathology. The key thing to the management of this problem, is to treat the person, not the scan or the pathology.
What are the symptoms of disc pathology?
As indicated above, symptoms are very variable. Disc pathology alone can cause pain in the back as well as referred pain into the limb. This type of pain is usually a dull, aching, toothache kind of pain. If nerve tissue is irritated, the pain is usually more severe, sharp and burning. It is often difficult for people with nerve pain to sleep due to the pain. Nerve irritation can sometimes result in pins and needles/tingling or numbness, and occasionally in sensations of weakness. Very rarely, if the disc pathology moves centrally towards the spinal cord, it can compress the nerves that supply your bladder and bowel and can effect sexual function. This is called Cauda Equina Syndrome and although it is very rare, it is a very serious condition that requires immediate medical attention.
What can cause a disc pathology?
The truth is – we don’t really know. As we have said – lots of people without back pain have disc pathology, so we need to be careful in saying you did this activity, you have pain and your spine shows evidence of disc pathology, therefore that is the cause. The pathology could have been there for a long time before the activity. In most cases, back pain is the result of a combination of factors that are unique to each individual. Research has shown that factors such as poor general fitness, fatigue, stress and sudden changes in activity levels (increases or decreases) are associated with back pain developing. It’s usually impossible to identify one precipitating factor – it’s more like a “perfect storm” – a combination of small, minor factors (each individually of no consequence) but when added together result in pain.
Treating disc pathology
The most important thing in treating back pain associated with disc pathology is to understand the information above about the pathology and its relationship to back pain. If you are reading this and have back pain, you should take this information to your health care professional, along with any questions you have, so that you can learn what is important in managing your pain and getting back to full function as quickly as possible.
Avoiding activity and lying/sitting down for long periods of time will only make matters worse. You should try and stay as active and mobile as possible, even if this requires medication for pain relief (Paracetamol, Aspirin, Ibuprofen) for a short period of time. Many people try to avoid pain relief, but it can be very beneficial in the short term to help you stay active and avoid a cycle of ongoing, constant pain. Always get advice on taking over-the-counter medication from a suitably qualified healthcare professional such as your GP, Practice Nurse, Pharmacist or Physiotherapist.
In the short term focus your active exercise on walking, cycling and gentle swimming.
Manual therapy can be beneficial for the management of symptoms, however, research has shown that manual therapy alone is very unlikely to have a long-lasting effect. Instead, we advise manual therapy in the initial stages alongside an individualised structured exercise program, designed just for you and prescribed by a qualified clinician. An effective programme should address specific problems you are having – flexibility, strength and your confidence with moving. Our spine is built to move and therefore it is important that we don’t focus too much on movements that don’t combine all 3 planes of movement in the spine (bending and extending, side bending and rotating). Gradually exposing yourself to all of these movements alongside a strength programme will ensure that symptoms don’t return. A combination of these things should be included in your programme to help you achieve effortless, pain-free movement. It is not just “core stability” that is important, and for many people, too much “core” work can make them worse – a bit like clenching your teeth too hard, for too long.
Should you symptoms not improve with physiotherapy management, you may be referred for an MRI scan to help guide the management. If there are signs of nerve compression on MRI that correlate to your symptoms and clinical assessment and things aren’t improving with the physiotherapy management then more invasive interventions may be advocated.
There is some research to support the use of steroid injections as part of the management of the symptoms of disc pathology, but this should only be considered if your pain has not improved with other elements of treatment. It is well documented that they should not be considered as providing a solution to pain, but in providing a window of opportunity to allow you to exercise effectively in order to achieve long-term relief. Some patients may also consider surgery as a treatment, however, 90% of herniated discs will resolve without surgical management, a very comforting figure if you are diagnosed with disc pathology as the cause to your symptoms. Surgery should only be considered in cases of Cauda Equina Syndrome or severe, unremitting symptoms with worsening neurological symptoms such as weakness.
Should your symptoms last longer than the expected healing time of an acute injury (around 6 weeks), and an MRI scan doesn’t show any structural cause to your symptoms that correlate with the clinical assessment, our bodies nervous system can become more sensitive to movements or activities that are perceived as harmful. Click here to read more about this.
To conclude, disc related pain can be a painful but completely treatable pathology. Ensuring you partake in regular exercise and knowing how to manage early symptoms, using the information explained above, will reduce the risk of more serious pain and dysfunction developing.
If you’re suffering from back pain, book an appointment to see one of our physiotherapists today.

Advice
Over the last 20+ years our experts have helped more than 100,000 patients, but we don’t stop there. We also like to share our knowledge and insight to help people lead healthier lives, and here you will find our extensive library of advice on a variety of topics to help you do the same.
OUR ADVICE HUBS See all Advice Hubs

