Pain Management
Our Consultants work with you to create a holistic management plan aimed at reducing your pain, enabling rehabilitation and enhancing your quality of life.

Pain can be a significant barrier to progression with a rehab program and hinder your ability to recover after an injury.

Our Pain Management Consultants understand the importance of a holistic approach to pain management, tailoring medication, interventional and therapeutic options in partnership with the patient in order to enable them to make the best recovery possible.
Book an appointmentPain Management Specialists

Pricing
- Initial Appointment (40 mins) – £350
- Follow-up Appointment (25 mins) – £250


Your initial appointment will include an expert assessment of your pain, the impact it has on your function and quality of life and outline the most appropriate treatment options available centring a management plan around your rehab goals.
Imaging such as MRI or CT SPECT scans can be seamlessly requested and used to inform your management plan which may include non-invasive, medicinal or interventional options.
Our Consultants are highly skilled at performing interventional pain management to provide targeted pain relief where required.
These include epidural steroid injections, diagnostic facet joint injections and radio frequency ablation, trigger point injections or peripheral nerve blocks.
Our Pain Management Consultants are completely integrated into your rehab team and are therefore perfectly placed to provide the most appropriate management to aid your return to fitness.
Pain Management can help
with conditions such as:
Back pain that persists despite non-surgical treatments, or where surgery is not indicated or desired, can still be effectively managed through a combination of conservative approaches. Physiotherapy plays a key role, using targeted exercises, manual therapy, and posture correction to reduce pain, improve mobility, and strengthen the supporting muscles of the spine. Other strategies such as pain management techniques, lifestyle modifications, and specialist input from osteopathy or rehabilitation professionals can also support long-term relief. A tailored, multidisciplinary approach offers a valuable alternative to surgery for many individuals living with chronic or unresolved back pain.
A disc prolapse, also known as a herniated or slipped disc, occurs when the soft inner gel of a spinal disc pushes through a tear in the tougher outer layer. This can irritate nearby nerves, leading to symptoms such as back pain, leg pain (sciatica), numbness, or weakness. Disc prolapses often occur in the lower back but can also affect the neck. While they can be painful, many cases improve with conservative treatments like physiotherapy, exercise, and pain management. In more severe or persistent cases, further medical or surgical intervention may be considered.
Spinal stenosis is a condition where the spaces within the spine narrow, putting pressure on the spinal cord and nerves. This narrowing typically occurs in the lower back or neck and can lead to symptoms like back pain, numbness, tingling, weakness, or difficulty walking. It is often caused by age-related changes, such as the thickening of ligaments or the development of bone spurs. While spinal stenosis can be managed with conservative treatments like physiotherapy, medication, and lifestyle changes, more severe cases may require surgical intervention to relieve pressure on the nerves and improve mobility.
Chronic pain is persistent pain that lasts for months or even years, often beyond the usual healing time of an injury or illness. It can be caused by a variety of factors, including ongoing conditions like arthritis, nerve damage, or back issues, and may also arise without any clear underlying cause. Unlike acute pain, which acts as a warning signal, chronic pain can affect a person’s daily life, leading to emotional, physical, and social challenges. Managing chronic pain typically involves a combination of treatments, including physical therapy, medication, lifestyle changes, and sometimes psychological support to help improve quality of life and reduce pain.
Acute pain is a sudden, sharp discomfort that typically results from an injury, illness, or surgery. It serves as a warning sign to the body that something is wrong and usually resolves once the underlying cause is treated or healed. Acute pain can be intense but is typically short-lived, lasting from a few seconds to several weeks. Common examples include pain from a sprained ankle, a broken bone, or a surgical procedure. Treatment for acute pain often involves pain relief methods such as medication, rest, ice, or physical therapy to promote healing and ease discomfort.
Coccygeal pain, also known as coccydynia, is discomfort or pain that occurs in the area around the tailbone (coccyx) at the base of the spine. It is often caused by injury, such as a fall, prolonged sitting on hard surfaces, or repetitive activities that strain the tailbone. Other potential causes include childbirth, infections, or underlying conditions like arthritis. The pain may worsen when sitting or standing up from a seated position, and it can range from a dull ache to sharp, intense discomfort. Treatment typically involves pain management, physical therapy to strengthen surrounding muscles, and adjustments to daily habits to reduce pressure on the coccyx.
Neck pain is a common condition that can result from a variety of causes, including poor posture, muscle strain, injury (such as whiplash), or degenerative conditions like arthritis. The pain can be localised to the neck or radiate to the shoulders, arms, or head, often accompanied by stiffness or headaches. It may be triggered by activities such as sitting at a desk for extended periods, sleeping in an awkward position, or engaging in repetitive motions. Treatment for neck pain often involves rest, heat or cold therapy, physical therapy, and posture correction, with more severe cases requiring medical interventions like medication or, in rare instances, surgery.
Widespread pain refers to discomfort that affects multiple areas of the body, often without a clear localised source. It is commonly associated with conditions like fibromyalgia, where the pain is chronic, dull, and may be accompanied by fatigue, sleep disturbances, and tenderness in specific “trigger points.” Widespread pain can also result from inflammatory disorders, stress, or injury. Unlike localised pain, which tends to affect one area, widespread pain involves a broader range of muscles, joints, or tissues, making it more challenging to manage. Treatment typically focuses on managing symptoms through a combination of medication, physical therapy, stress management, and lifestyle adjustments.
Neuropathic pain is a type of chronic pain caused by damage or dysfunction of the nerves themselves, rather than injury to tissues. It often feels like burning, tingling, shooting, or stabbing sensations and can be accompanied by numbness or hypersensitivity. This type of pain is commonly associated with conditions such as diabetes (diabetic neuropathy), shingles (postherpetic neuralgia), multiple sclerosis, or nerve injuries. Neuropathic pain can be difficult to treat, as it doesn’t respond well to standard pain relievers. Treatment typically involves medications like anticonvulsants or antidepressants, physical therapy, and sometimes nerve blocks or other specialised therapies to manage symptoms.
Complex Regional Pain Syndrome (CRPS) is a chronic pain condition that typically affects a limb after an injury, with pain that is more intense and prolonged than expected. The pain is often accompanied by changes in skin colour, temperature, swelling, and sensitivity, and may spread beyond the initial injury site. CRPS is thought to result from dysfunction in the nervous system, causing an exaggerated response to injury and affecting both sensory and motor functions. It can be challenging to treat, and management usually involves a multidisciplinary approach, including physical therapy, pain management, and sometimes medications or nerve blocks, to help reduce pain and improve movement.
Post-traumatic pain is pain that persists after an injury or trauma, often continuing long after the initial injury has healed. This type of pain can result from physical damage to tissues, nerves, or bones, but it can also arise from psychological factors, such as emotional stress or anxiety related to the trauma. The pain may be localised to the area of injury or more widespread and can be acute or chronic in nature. Treatment typically involves a combination of pain management techniques, physical therapy, psychological support, and sometimes medications to address both the physical and emotional aspects of the pain.
Post-surgical pain is the discomfort that occurs after undergoing a surgical procedure, resulting from the trauma caused by incisions, tissue manipulation, or the body’s natural healing response. This type of pain can vary in intensity, ranging from mild soreness to more severe, throbbing sensations, and typically peaks within the first few days after surgery. While post-surgical pain usually decreases as the body heals, it can persist for weeks or months in some cases. Management often involves a combination of pain medications, physical therapy, and rest, with the goal of reducing discomfort and supporting the recovery process.
Post-amputation pain refers to the discomfort experienced after the loss of a limb, which can be both physical and emotional. It often includes phantom limb pain, where the individual feels sensations in the missing limb, such as itching, burning, or cramping, despite the limb no longer being present. There may also be residual limb pain in the remaining part of the limb, caused by factors like pressure, irritation, or inflammation. This type of pain can be chronic and difficult to manage, requiring a combination of treatments such as medication, physical therapy, desensitisation techniques, and psychological support to improve quality of life and help the person adapt to the changes.
Sciatica is a condition characterised by pain that radiates along the sciatic nerve, which runs from the lower back, through the hips, and down each leg. It typically occurs when the nerve is compressed or irritated, often due to a herniated disc, spinal stenosis, or muscle tension. The pain can range from mild to severe and may be accompanied by numbness, tingling, or weakness in the affected leg. Sciatica often worsens with activities like sitting, standing, or lifting. Treatment typically includes physical therapy, pain management, and lifestyle adjustments to relieve pressure on the nerve, with surgery considered in more severe cases.
Chronic knee pain is persistent discomfort that lasts for months or even years, often due to conditions like osteoarthritis, tendinitis, or previous injuries such as ligament tears. It can also result from overuse, muscle imbalances, or structural issues in the knee joint. Symptoms typically include aching, stiffness, swelling, and difficulty with movement or weight-bearing activities like walking or climbing stairs. Managing chronic knee pain often involves a combination of physical therapy to strengthen the muscles around the knee, pain management, lifestyle modifications, and in some cases, injections or surgery to address underlying issues.
Your guide to Pain Management at Pure
Your body is your most important investment, and it deserves more. Make sure you get the tailored care and treatment your individual case requires.

-
Work with a dedicated team of specialists, tailored to meet your specific needs and goals.
-
We combine over 1,000 years of expert experience in musculoskeletal healthcare and elite sport.
-
We are covered by all major insurers and also offer flexible self-pay options for added convenience.
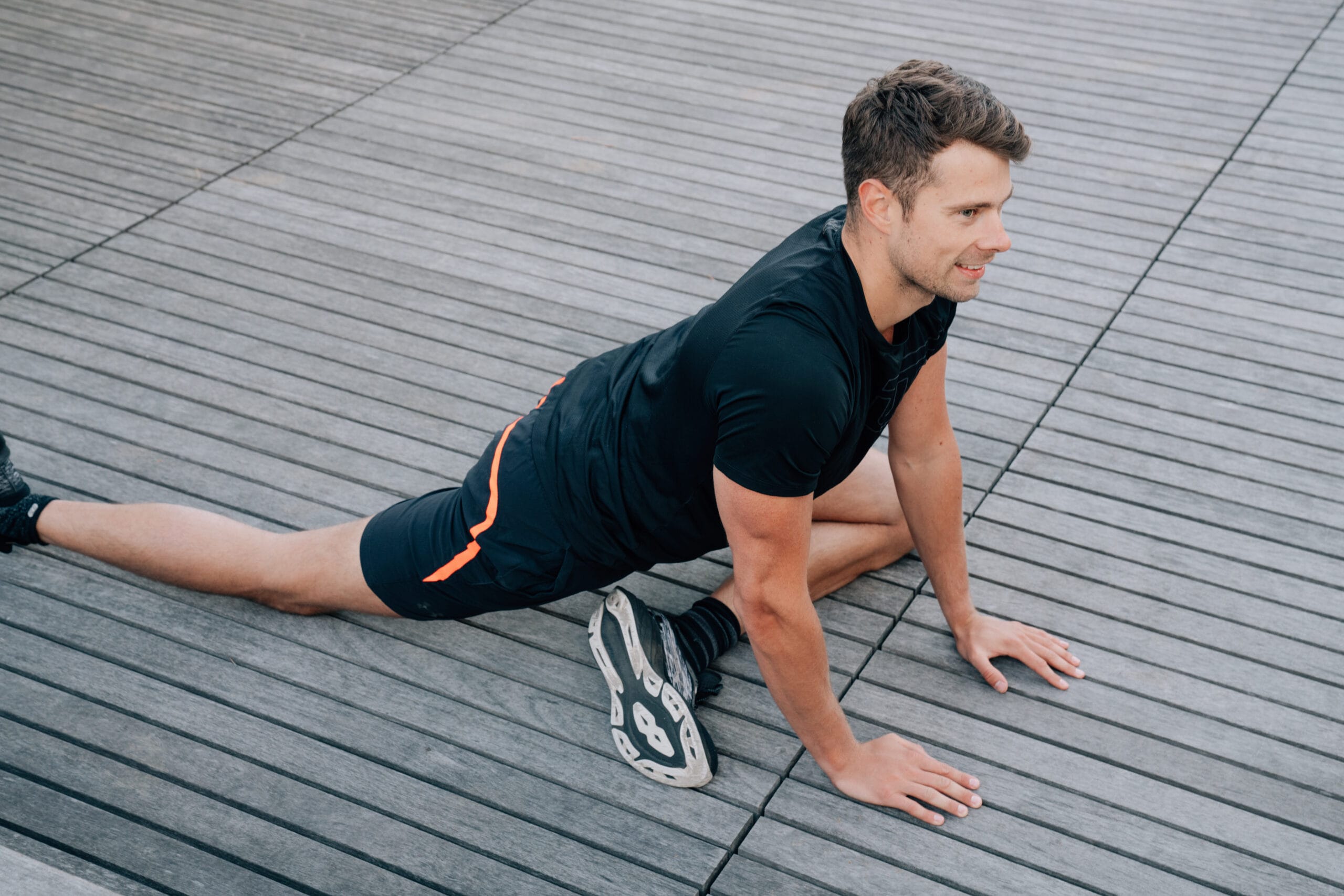
Your Journey with Pure
Everything we do is personalised to you. Whether your goal is to run a marathon or simply walk up the stairs comfortably, we’ll deliver the correct diagnosis and tailored treatment you need to get there so that you can perform at your best and prevent reoccurrence.

Treatments can include:
- Medication review
- Epidural injection
- Facet joint injections
- Radiofrequency ablation
- Trigger point injections
- Joint injection
- Sacroiliac joint injection
- Coccygeal joint injections
- Peripheral nerve blocks